A public awareness article on Parkinson published courtesy of Mayo Clinic Minnesota, United States
What is Parkinson disease?
Parkinson disease is a progressive disorder of the nervous system that affects movement. It develops gradually, sometimes starting with a barely noticeable tremor in just one hand. But while a tremor may be the most well-known sign of Parkinson’s disease, the disorder also commonly causes stiffness or slowing of movement.
In the early stages of Parkinson’s disease, your face may show little or no expression, or your arms may not swing when you walk. Your speech may become soft or slurred. Parkinson’s disease symptoms worsen as your condition progresses over time.
Although Parkinson’s disease can’t be cured, medications may markedly improve your symptoms. In occasional cases, your doctor may suggest surgery regulate certain regions of your brain and improve your symptoms.
Symptoms
By Mayo Clinic Staff
Parkinson’s disease symptoms and signs may vary from person to person. Early signs may be mild and may go unnoticed. Symptoms often begin on one side of your body and usually remain worse on that side, even after symptoms begin to affect both sides.
Parkinson’s signs and symptoms may include:
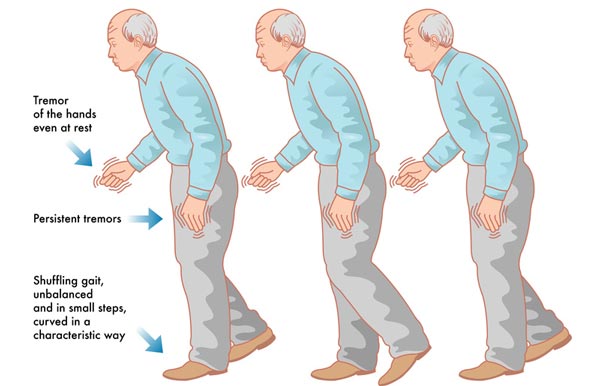
- A tremor, or shaking, usually begins in a limb, often your hand or fingers. You may notice a back-and-forth rubbing of your thumb and forefinger, known as a pill-rolling tremor. One characteristic of Parkinson’s disease is a tremor of your hand when it is relaxed (at rest).
- Slowed movement (bradykinesia). Over time, Parkinson’s disease may reduce your ability to move and slow your movement, making simple tasks difficult and time-consuming. Your steps may become shorter when you walk, or you may find it difficult to get out of a chair. Also, you may drag your feet as you try to walk, making it difficult to move.
- Rigid muscles. Muscle stiffness may occur in any part of your body. The stiff muscles can limit your range of motion and cause you pain.
- Impaired posture and balance. Your posture may become stooped, or you may have balance problems as a result of Parkinson’s disease.
- Loss of automatic movements. In Parkinson’s disease, you may have a decreased ability to perform unconscious movements, including blinking, smiling, or swinging your arms when you walk.
- Speech changes. You may have speech problems as a result of Parkinson’s disease. You may speak softly, quickly, slur, or hesitate before talking. Your speech may be more of a monotone rather than with the usual inflections.
- Writing changes. It may become hard to write, and your writing may appear small.
When to see a doctor
See your doctor if you have any of the symptoms associated with Parkinson’s disease — not only to diagnose your condition but also to rule out other causes for your symptoms
In Parkinson’s disease, certain nerve cells (neurons) in the brain gradually break down or die. Many of the symptoms are due to a loss of neurons that produce a chemical messenger in your brain called dopamine. When dopamine levels decrease, it causes abnormal brain activity, leading to signs of Parkinson’s disease.
The cause of Parkinson’s disease is unknown, but several factors appear to play a role, including:
- Your genes. Researchers have identified specific genetic mutations that can cause Parkinson’s disease, but these are uncommon except in rare cases with many family members affected by Parkinson’s disease.
However, certain gene variations appear to increase the risk of Parkinson’s disease but with a relatively small risk of Parkinson’s disease for each of these genetic markers.
- Environmental triggers. Exposure to certain toxins or environmental factors may increase the risk of later Parkinson’s disease, but the risk is relatively small.
Researchers have also noted that many changes occur in the brains of people with Parkinson’s disease, although it’s not clear why these changes occur. These changes include:
- The presence of Lewy bodies. Clumps of specific substances within brain cells are microscopic markers of Parkinson’s disease. These are called Lewy bodies, and researchers believe these Lewy bodies hold an important clue to the cause of Parkinson’s disease.
- Alpha-synuclein is found within Lewy bodies. Although many substances are found within Lewy bodies, scientists believe an important one is a natural and widespread protein called alpha-synuclein (A-synuclein). It’s found in all Lewy bodies in a clumped form that cells can’t break down. This is currently an important focus among Parkinson’s disease researchers.
Complications
By Mayo Clinic Staff
Parkinson’s disease is often accompanied by these additional problems, which may be treatable:
- Thinking difficulties. You may experience cognitive problems (dementia) and thinking difficulties, which usually occur in the later stages of Parkinson’s disease. Such cognitive problems aren’t very responsive to medications.
- Depression and emotional changes. People with Parkinson’s disease may experience depression. Receiving treatment for depression can make it easier to handle the other challenges of Parkinson’s disease.
You may also experience other emotional changes, such as fear, anxiety, or loss of motivation. Doctors may give you medications to treat these symptoms.
- Swallowing problems. You may develop difficulties with swallowing as your condition progresses. Saliva may accumulate in your mouth due to slowed swallowing, leading to drooling.
- Sleep problems and sleep disorders. People with Parkinson’s disease often have sleep problems, including waking up frequently throughout the night, waking up early, or falling asleep during the day.
People may also experience rapid eye movement sleep behavior disorder, which involves acting out your dreams. Medications may help your sleep problems.
- Bladder problems. Parkinson’s disease may cause bladder problems, including being unable to control urine or having difficulty urinating.
- Many people with Parkinson’s disease develop constipation, mainly due to a slower digestive tract.
You may also experience:
- Blood pressure changes. You may feel dizzy or lightheaded when you stand due to a sudden drop in blood pressure (orthostatic hypotension).
- Smell dysfunction. You may experience problems with your sense of smell. You may have difficulty identifying certain odors or the difference between odors.
- Many people with Parkinson’s disease lose energy and experience fatigue, and the cause isn’t always known.
- Many people with Parkinson’s disease experience pain, either in specific areas of their bodies or throughout their bodies.
- Sexual dysfunction. Some people with Parkinson’s disease notice a decrease in sexual desire or performance.
f you’ve received a diagnosis of Parkinson’s disease, you’ll need to work closely with your doctor to find a treatment plan that offers you the greatest relief from symptoms with the fewest side effects. Certain lifestyle changes may also help make living with Parkinson’s disease easier.
Healthy eating
While there’s no food or combination of foods proven to help in Parkinson’s disease, some foods may help ease some of the symptoms. For example, eating foods high in fiber and drinking an adequate amount of fluids can help prevent constipation that is common in Parkinson’s disease.
A balanced diet also provides nutrients, such as omega-3 fatty acids, that may be beneficial for people with Parkinson’s disease.
Exercise
Exercising may increase your muscle strength, flexibility, and balance. Exercise can also improve your well-being and reduce depression or anxiety.
Your doctor may suggest you work with a physical therapist to learn an exercise program that works for you. You may also try exercises such as walking, swimming, gardening, dancing, water aerobics or stretching.
Parkinson’s disease can disturb your sense of balance, making it difficult to walk with a normal gait. Exercise may improve your balance. These suggestions may also help:
- Try not to move too quickly.
- Aim for your heel to strike the floor first when you’re walking.
- If you notice yourself shuffling, stop and check your posture. It’s best to stand up straight.
- Look in front of you, not directly down, while walking.
Avoiding falls
In the later stages of the disease, you may fall more easily. In fact, you may be thrown off balance by just a small push or bump. The following suggestions may help:
- Make a U-turn instead of pivoting your body over your feet.
- Distribute your weight evenly between both feet, and don’t lean.
- Avoid carrying things while you walk.
- Avoid walking backward.
Daily living activities
Daily living activities — such as dressing, eating, bathing, and writing — can be difficult for people with Parkinson’s disease. An occupational therapist can show you techniques that make daily life easier.
Coping and support
By Mayo Clinic Staff
Living with any chronic illness can be difficult, and it’s normal to feel angry, depressed or discouraged at times. Parkinson’s disease, in particular, can be profoundly frustrating, as walking, talking, and even eating become more difficult and time-consuming.
Depression is common in people with Parkinson’s disease. But antidepressant medications can help ease the symptoms of depression, so talk with your doctor if you’re feeling persistently sad or hopeless.
Although friends and family can be your best allies, the understanding of people who know what you’re going through can be especially helpful. Support groups aren’t for everyone. However, for many people with Parkinson disease and their families, support groups can be a good resource for practical information about Parkinson’s disease.
Also, groups offer a place for you to find people who are going through similar situations and can support you.
To learn about support groups in your community, talk to your doctor, a Parkinson disease social worker, or a local public health nurse. Or contact the National Parkinson Foundation or the American Parkinson Disease Association.
You and your family may also benefit from talking to a mental health professional (psychologist) or social worker trained in working with people who have chronic conditions.
Because the cause of Parkinson’s is unknown, proven ways to prevent the disease also remain a mystery. However, some research has shown that caffeine — which is found in coffee, tea, and cola — may reduce the risk of developing Parkinson’s disease. Green tea also may reduce the risk of developing Parkinson’s disease.
Some research has shown that regular aerobic exercise may reduce the risk of Parkinson disease.
Courtesy by: http://www.mayoclinic.org/diseases-conditions/parkinsons-disease/basics/definition/con-20028488
References
- Longo DL, et al. Parkinson’s disease and other movement disorders. In: Harrison’s Principles of Internal Medicine. 18th ed. New York, N.Y.: The McGraw-Hill Companies; 2012. http://accessmedicine.com. Accessed April 6, 2015.
- Parkinson’s disease: Hope through research. National Institute of Neurological Disorders and Stroke. http://www.ninds.nih.gov/disorders/parkinsons_disease/detail_parkinsons_disease.htm. Accessed April 6. 2015.
- Ferri FF. Parkinson’s disease. In: Ferri’s Clinical Advisor 2015: 5 Books in 1. Philadelphia, Pa.: Mosby Elsevier; 2015. https://www.clinicalkey.com. Accessed April 6, 2015.
- Chou KL. Diagnosis of Parkinson’s disease. http://www.uptodate.com/home. Accessed April 6. 2015.
- Tarsy D. Pharmacologic treatment of Parkinson’s disease. http://www.uptodate.com/home. Accessed April 6. 2015.
- Adler CH, et al. Submandibular gland needle biopsy for the diagnosis of Parkinson’s disease. Neurology. 2014;82:858.
- Bousquet M, et al. Impact of omega-3 fatty acids in Parkinson’s disease. Ageing Research Reviews. 2011;10:453.
- Parkinson’s disease: Fitness counts. National Parkinson Foundation. http://www.parkinson.org/Search-Pages/Search.aspx?pKeywords=fitness. Accessed April 9, 2015.
- Parkinson’s disease. Natural Medicines Comprehensive Database. http://www.naturaldatabase.com. Accessed April 6, 2015.
- Tarsy D. Nonpharmacologic management of Parkinson’s disease. http://www.uptodate.com/home/. Accessed April 6, 2015.
- Complementary therapies and Parkinson’s. Parkinson’s Disease Society of the United Kingdom. http://www.parkinsons.org.uk/content/complementary-therapies-and-parkinsons-booklet. Accessed April 9, 2015.
- Jankovic J. Etiology and pathogenesis of Parkinson’s disease. http://www.uptodate.com/home. Accessed April 6, 2015.
- Riggs EA. Decision Support System. Mayo Clinic, Rochester, Minn. April 16, 2015.
- Abbvie announces U.S. approval of drop (carbidopa and levodopa) enteral suspension for the treatment of motor fluctuations in patients with advanced Parkinson’s disease. http://abbvie.mediaroom.com/2015-01-12-AbbVie-Announces-U-S-FDA-Approval-of-DUOPA-carbidopa-and-levodopa-Enteral-Suspension-for-the-Treatment-of-Motor-Fluctuations-in-Patients-with-Advanced-Parkinsons-Disease. Accessed April 20, 2015.
Bower JH (expert opinion). Mayo Clinic, Rochester, Minn. April 20, 2015.


 Reach us on WhatsApp
Reach us on WhatsApp